allergic rhinitis or hay fever
allergic rhinitis or hay fever
Rhinitis is broadly defined as inflammation of the nasal mucosa. It is a common disorder that affects up to 40% of the population. Allergic rhinitis is the most common type of chronic rhinitis, affecting 10 to 20% of the population, and evidence suggests that the prevalence of the disorder is increasing. Severe allergic rhinitis has been associated with significant impairments in quality of life, sleep and work performance.
In the past, allergic rhinitis was considered to be a disorder localized to the nose and nasal passages, but current evidence indicates that it may represent a component of systemic airway disease involving the entire respiratory tract. There are a number of physiological, functional and immunological relationships between the upper (nose, nasal cavity, paranasal sinuses, pharynx, and larynx) and lower (trachea, bronchial tubes, bronchioles, and lungs) respiratory tracts. For example, both tracts contain a ciliated epithelium consisting of goblet cells that secrete mucous, which serves to filter the incoming air and protect structures within the airways. Furthermore, the submucosa of both the upper and lower airways includes a collection of blood vessels, mucous glands, supporting cells, nerves and inflammatory cells. Evidence has shown that allergen provocation of the upper airways not only leads to a local inflammatory response, but also to inflammatory processes in the lower airways, and this is supported by the fact that rhinitis and asthma frequently coexist. Therefore, allergic rhinitis and asthma appear to represent a combined airway inflammatory disease, and this needs to be considered to ensure the optimal assessment and management of patients with allergic rhinitis.
Comprehensive and widely-accepted guidelines for the diagnosis and treatment of allergic rhinitis were published in 2007. This article provides an overview of the recommendations provided in these guidelines as well as a review of current literature related to the pathophysiology, diagnosis, and appropriate management of allergic rhinitis.
Rhinitis is classified into one of the following categories according to etiology: IgE-mediated (allergic), autonomic, infectious and idiopathic (unknown). Although the focus of this article is allergic rhinitis, a brief description of the other forms of rhinitis is provided in Table 1.
Etiological classification of rhinitis.
Description
| |
|---|---|
IgE-mediated (allergic)
|
• IgE-mediated inflammation of the nasal mucosa, resulting in eosinophilic and Th2-cell infiltration of the nasal lining
• Further classified as intermittent or persistent
|
Autonomic
|
• Drug-induced (rhinitis medicamentosa)
• Hypothyroidism
• Hormonal
• Non-allergic rhinitis with eosinophilia syndrome (NARES)
|
Infectious
|
• Precipitated by viral (most common), bacterial, or fungal infection
|
Idiopathic
|
• Etiology cannot be determined
|
Allergic rhinitis is usually a long-standing condition that often goes undetected in the primary-care setting. Patients suffering from the disorder often fail to recognize the impact of the disorder on quality of life and functioning and, therefore, do not frequently seek medical attention. In addition, physicians fail to regularly question patients about the disorder during routine visits.T herefore, screening for rhinitis is recommended, particularly in asthmatic patients since studies have shown that rhinitis is present in up to 95% of patients with asthma.
A thorough history and physical examination are the cornerstones of establishing the diagnosis of allergic rhinitis. Allergy testing is also important for confirming that underlying allergies cause the rhinitis. Referral to an allergist should be considered if the diagnosis of allergic rhinitis is in question.
Components of a complete history and physical examination for suspected rhinitis.
History
|
Physical examination
|
|---|---|
Personal
• Nasal itch
• Rhinorrhea
• Sneezing
• Eye involvement
• Seasonality
• Triggers
Family
• Allergy
• Asthma
Environmental
• Pollens
• Animals
• Flooring/upholstery
• Mould
• Humidity
• Tobacco exposure
Medication/drug use
• Beta-blockers
• ASA
• NSAIDs
• ACE inhibitors
• Hormone therapy
• Recreational cocaine use
Quality of life
• Rhinitis-specific questionnaire
Comorbidities
• Asthma
• Mouth breathing
• Snoring
• Sinus involvement
• Otitis media
• Nasal polyps
• Conjunctivitis
Response to previous medications
• Second-generation oral antihistamines
• Intranasal corticosteroids
|
Outward signs
• Mouth breathing
• Rubbing the nose/transverse nasal crease
• Frequent sniffling and/or throat clearing
• Allergic shiners (dark circles under eyes)
Nose
• Mucosal swelling, bleeding
• Pale, thin secretions
• Polyps or other structural abnormalities
Ears
• Generally normal
• Pneumatic otoscopy to assess for Eustachian tube dysfunction
• Valsalva’s maneuver to assess for fluid behind the ear drum
Sinuses
• Palpation of sinuses for signs of tenderness
• Maxillary tooth sensitivity
Posterior oropharynx
• Postnasal drip
• Lymphoid hyperplasia (“cobblestoning”)
• Tonsillar hypertrophy
Chest and skin
• Atopic disease
• Wheezing
|
Diagnostic tests
Although a thorough history and physical examination are required to establish the clinical diagnosis of rhinitis, further diagnostic testing is usually necessary to confirm that underlying allergies cause the rhinitis. Skin-prick testing is considered the primary method for identifying specific allergic triggers of rhinitis. Skin prick testing involves placing a drop of a commercial extract of a specific allergen on the skin of the forearms or back, then pricking the skin through the drop to introduce the extract into the epidermis. Within 15-20 minutes, a wheal-and-flare response (an irregular blanched wheal surrounded by an area of redness) will occur if the test is positive. Testing is typically performed using the allergens relevant to the patient’s environment (e.g., pollen, animal dander, moulds and house dust mites). A reasonable alternative to skin prick testing is the use of allergen-specific IgE tests (e.g., radioallergosorbent tests [RASTs]) that provide an in vitro measure of a patient’s specific IgE levels against particular allergens. However, skin prick tests are generally considered to be more sensitive and cost-effective than allergen-specific IgE tests, and have the further advantage of providing physicians and patients with immediate resultsTreatment
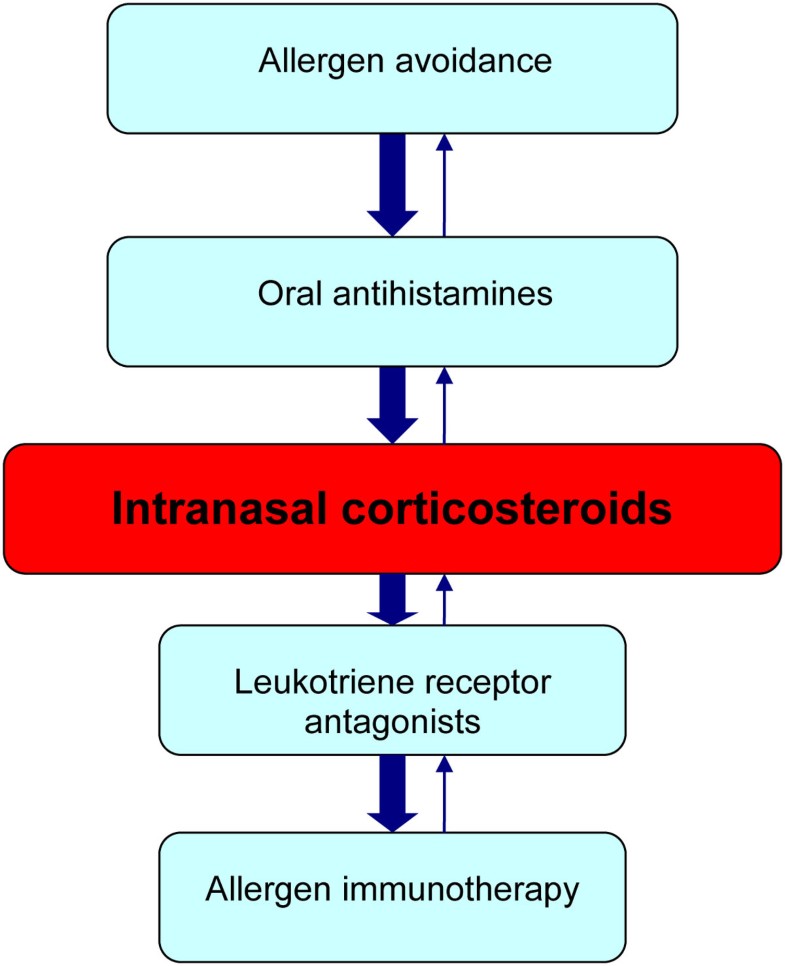
The treatment goal for allergic rhinitis is relief of symptoms. Therapeutic options available to achieve this goal include avoidance measures, oral antihistamines, intranasal corticosteroids, leukotriene receptor antagonists, and allergen immunotherapy. Other therapies that may be useful in select patients include decongestants and oral corticosteroids. If the patient’s symptoms persist despite appropriate treatment, referral to an allergist should be considered. As mentioned earlier, allergic rhinitis and asthma appear to represent a combined airway inflammatory disease and, therefore, treatment of asthma is also an important consideration in patients with allergic rhinitis.
Usual adult dose
|
Usual pediatric dose
| |
|---|---|---|
Oral antihistamines (second generation)
| ||
Cetirizine (Reactine)
|
1-2 tablets (5 mg) once daily
1 tablet (10 mg) once daily
|
5-10 mL (1-2 teaspoons) once daily (children’s formulation)
|
Desloratadine (Aerius)
|
1 tablet (5 mg), once daily
|
2.5-5 mL (0.5-1.0 teaspoon) once daily (children’s formulation)
|
Fexofenadine (Allegra)
|
1 tablet (60 mg) every 12 hours (12-hour formulation)
1 tablet (120 mg), once daily (24-hour formulation)
|
Not currently indicated for children under 12 years of age
|
Loratadine (Claritin)
|
1 tablet (10 mg), once daily
|
5-10 mL (1-2 teaspoons) once daily (children’s formulation)
|
Intranasal corticosteroids
| ||
Beclomethasone (Beconase)
|
1-2 sprays (42 µg/spray) EN, twice daily
|
1 spray (42 µg/spray) EN, twice daily
|
Budesonide (Rhinocort)
|
2 sprays (64 μg/spray) EN, once daily or 1 spray EN, twice daily
|
2 sprays (64 μg/spray) EN, once daily or 1 spray EN, twice daily (do not exceed 256 μg)
|
Ciclesonide (Omnaris)
|
2 sprays (50 µg/spray) EN, once daily
|
Not indicated for children under 12 years of age
|
Fluticasone furoate (Avamys)
|
2 sprays (27.5 µg/spray) EN, once daily
|
1 spray (27.5 µg/spray) EN, once daily
|
Fluticasone propionate (Flonase)
|
2 sprays (50 µg/spray) EN, once daily or every 12 hours (for severe rhinitis)
|
1-2 sprays (50 µg/spray) EN, once daily
|
Mometasone furoate (Nasonex)
|
2 sprays (50 µg/spray) EN, once daily
|
1 spray (50 µg/spray) EN, once daily
|
Triamcinolone acetonide (Nasacort)
|
2 sprays (55 µg/spray) EN, once daily
|
1 spray (55 µg/spray) EN, once daily
|
Leukotriene receptor antagonists
| ||
Montelukast
|
1 tablet (10 mg), once daily
|
Not currently approved for patients under 15 years of age
|










No comments